More Than Telehealth: Social Factors Shape Heart Health
Heart health tied not just to habits, but to access and opportunity, study finds
OXFORD, Miss. – A team of researchers led by two University of Mississippi professors is working to unlock patterns and causes of the No. 1 killer of Mississippians: heart disease.
Ruaa Al Juboori, assistant professor of public health and data analytics statistician, and Andrew Yockey, assistant professor of public health, analyzed data from 418 counties in Alabama, Georgia, Louisiana, Mississippi and South Carolina. They used mapping and statistical methods to test hypotheses, explore patterns in heart disease rates, and identify key social and structural factors linked to those patterns.
They found that especially high rates of coronary heart disease, or CHD, deaths were found in the Mississippi Delta and parts of western Alabama. These areas often face challenges such as poverty, shortages of health care workers and ongoing health inequalities.

"One of the most promising findings from our spatial analysis was the protective role of health care provider availability, particularly primary care physicians, on coronary heart disease outcomes," said Al Juboori, lead author of the study that was published in the International Journal of Environmental Research and Public Health.
The results indicate that even small increases in the number of primary care physicians in an area can produce a substantial improvement in CHD rates and mortality, she said.
"This highlights the impact that even modest investments in rural health care workforce capacity, through initiatives like loan forgiveness programs or rural residency incentives, could have on improving cardiovascular health," Al Juboori said.
Not all Southern regions were ranked poorly. In fact, some performed better than expected, she said.
"Despite facing structural disadvantages such as low broadband access, high rurality and economic hardship, Washington County, Alabama, stood out in this regard," Al Juboori said. "Despite limited provider density and a high proportion of households without digital access or vehicles, the county reported lower-than-expected CHD mortality."
Treutlen County, Georgia, also stood out with better-than-expected cardiovascular outcomes despite structural challenges, said Neva Agarwala, a researcher at South College and a co-author of the study.
"This may reflect state-supported efforts like the Georgia Rural Health Innovation Center, which expanded telehealth access to over 130 rural clinics," Agarwala said. "The Georgia Department of Public Health also deploys community health workers to provide chronic disease education and support in underserved areas."
"These initiatives help reduce access barriers and promote better health outcomes in rural communities."
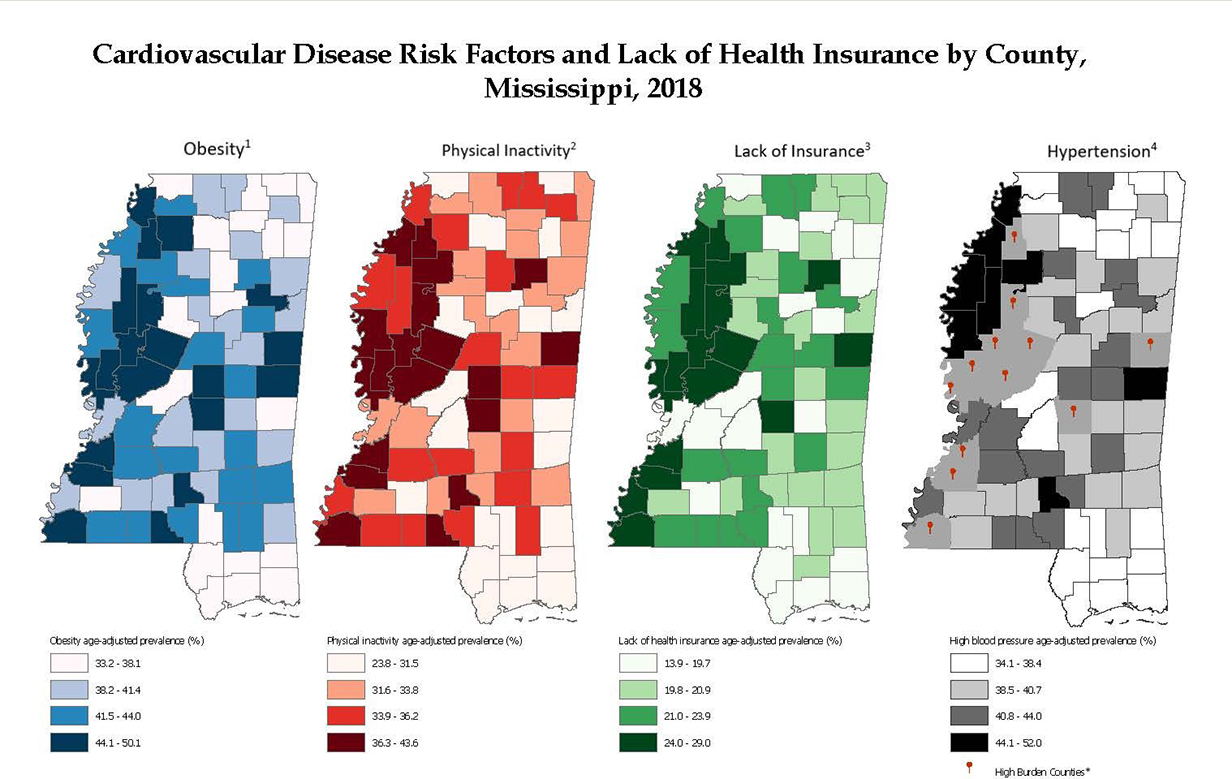
Social and lifestyle factors that influence the risk of cardiovascular disease vary by county across Mississippi and surrounding states. Graphic by Mississippi Department of Health
A key takeaway from this study is that not all rural areas face the same challenges, Al Juboori said. Some counties have overlapping barriers including low income, aging populations and no access to providers or digital tools, while others may have strengths to build on.
This study revealed that closing the digital divide is essential for expanding telehealth in rural areas.
"In the Deep South counties we studied, approximately 10.3% of households lacked a computer or smartphone, and broadband infrastructure was still underdeveloped in many areas, especially compared to national averages," Al Juboori said. "This means that even where broadband is technically available, many residents are still unable to use telehealth due to affordability or lack of digital readiness."
But technology alone is not enough, she said.
"Telehealth needs to be paired with strong local health care infrastructure," she explained. "Mobile clinics and community health workers can help bridge the gap. Ultimately, telehealth can be part of a hybrid care model that combines digital tools with community-based support."
Yockey suggested that taking inspiration from regions in the West where heart disease rates are especially low can be a good idea.

"Denver, Colorado is a resilient county because everyone is healthy and they have resources," he said. "The cost of living is a little higher, but they have more things to better promote health and social well-being than Mississippi."
According to South Denver Cardiology, Colorado has the third-lowest heart disease rate in the country, the fifth-lowest number of heart disease deaths per 100,000 adults between 45 and 64, and the highest percentage of physically active adults in the country.
"Studying resilient counties with favorable outcomes that outperform expectations can help identify scalable, community-driven strategies to improve health equity," said J. Riley Morgan, of Tupelo, who earned a master's degree in public health in 2024.
Morgan was among several Ole Miss graduate students in public health who assisted with the study. He helped review literature on telehealth and health access in the Deep South.
"Improving health access in Mississippi's rural regions could also reduce long-term health care costs, increase workforce participation and strengthen the state's economy by keeping more residents healthy and able to work," he said.
By 2030, the state will need an additional 364 primary care providers, 24% more than the 2010 workforce, to meet the demands of an aging, growing and increasingly insured population, according to the Robert Graham Center.
"You look at Mississippi – 82 counties, and 80 of them have major health care disparities," Yockey said. "For example, 12 counties in Mississippi have been identified as 'high burden' for cardiovascular disease risk – meaning they rank in the top 25% statewide for obesity, physical inactivity, hypertension and have the lowest levels of health insurance coverage. There's a clear issue.
"I grew up in a very rural environment, so having a rural health care approach really matters. We need a program that blends metropolitan and rural health. Rural counties are being neglected, no matter where you are."
Top: Heart disease is the No. 1 killer for Mississippians, but a UM study indicates that communities can substantially improve their rates for cardiovascular disease and mortality by attracting more primary care physicians and investing in public health programs. Illustration by John McCustion/University Marketing and Communications
By
Jordan Karnbach
Campus
Office, Department or Center
Published
July 21, 2025
